Written by Dr Daniel J Nightingale.
Every 3 seconds someone in the world is diagnosed with a primary form of dementia. This may be a child, a young adult, or a senior member of society. It does not discriminate between class, race, or gender and affects people living in rural, urban, and suburban communities. It takes an entire village to support someone through their journey and currently, worldwide, there are over 50 million people being supported along this journey.
What is Dementia?
This is an umbrella term meaning a set of symptoms. Though used in general language, clinically we prefer to call it a neurocognitive disorder. For example, a correct diagnosis might be a Neurocognitive disorder of the Alzheimer type. This removes any loose terminology such as ‘pleasantly confused’ and other terms that I regard as being a personal detractor. There are over 100 types of dementia, with Alzheimer’s disease, Vascular Dementia and Lewy Body type dementia being the most common. As I write this blog, there is no cure for Alzheimer’s disease or the other main types of dementia. There are some medicines whose primary function is to slow down the progression of the disease, but they are short acting and not suitable for everyone.
Available treatment and therapies
When discussing current treatment and therapies for people who have been diagnosed with a neurocognitive disorder such as Alzheimer’s disease, it is useful to consider both the medical and psychosocial models. The Medical Model is a term first coined by a psychiatrist called R D Laing and relates to the set of procedures in which all doctors are trained. These procedures are initial complaint, history, physical examination, lab tests where indicated, diagnosis, treatment, and prognosis. In terms of a neurocognitive dementia, it is important to assess the cognition of the individual as well as any physical and psychiatric symptoms. Brain scans and lab tests a part of this process. Once it is determined that the person has, for example, neurocognitive disorder of the Alzheimer’s type, the following medications are available:
- Cholinesterase inhibitors. These medications — including donepezil (Aricept), rivastigmine (Exelon) and galantamine (Razadyne) — work by boosting levels of a chemical messenger involved in memory and judgment. Although primarily used to treat Alzheimer’s disease, these medications might also be prescribed for other dementias, including vascular dementia, Parkinson’s disease dementia and Lewy body dementia. Side effects can include nausea, vomiting and diarrhea. Other possible side effects include slowed heart rate, fainting and sleep disturbances.
- Memantine. Memantine (Namenda) works by regulating the activity of glutamate, another chemical messenger involved in brain functions, such as learning and memory. In some cases, memantine is prescribed with a cholinesterase inhibitor.
- A common side effect of memantine is dizziness.
- Other medications. The doctor might prescribe medications to treat other symptoms or conditions, such as depression, sleep disturbances, hallucinations, parkinsonism, or agitation.
The psychosocial model views individuals in the context of a combination of influences that psychological factors and the surrounding social environment have on their physical and mental health and well-being and their ability to function. Examples include social support, loneliness, marital or relationship status, social disruption, bereavement, work environment, social status, and social integration.
When we think about those things in terms of someone living with Alzheimer’s disease or other neurocognitive disorder, all these factors, and more, are important considerations. As stated above, it is a journey shared by everyone.
When considering the Behavioural and Psychological Symptoms of Dementia (BPSD), which include disturbed perception, thought content, mood or behaviour that frequently occur as part of the day to day challenges, we must also consider the elements that fuel and exacerbate these symptoms. Two key fuels are the emotions of fear and anxiety. The diagram below demonstrates the negative impact that these have on the individual:
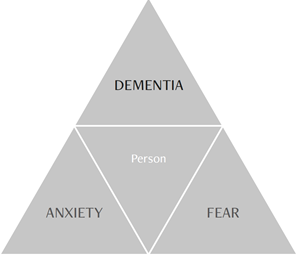
In the diagram above, we see DEMENTIA as the central player; the commander over the individual’s life and everything that happens. DEMENTIA has two allies: FEAR and ANXIETY. Together, they form the dementia triangle that fuels the disease and reduces every aspect of quality of life. This person, is slowly diminishing; becoming a shrinking violet with reduced confidence and self-esteem; withdrawing into a shell; becoming a shadow of their former self. Night after night, the person lives in constant FEAR. Every action is surrounded by high states of ANXIETY. Unless, through therapy, things change, the person, will not be able to live well with dementia. Gradually, he/she will become more and more diminished, more and more disempowered until end of life comes; and this comes much quicker than it needs to.
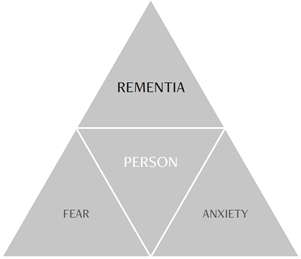
In the diagram above, we can see how supporting the person through an appropriate intervention, in this case, hypnotherapy for one hour a week for six weeks, there has been a positive change. It is at this juncture that the PERSON and the Nightingale Dementia Consultant have raged war against FEAR and ANXIETY. DEMENTIA is no longer the commander. Instead, the PERSON has taken centre stage. We have managed to transform a malignant life of dementia into a productive life of REMENTIA. Rementia is defined as ‘the regaining of lost cognitive functional abilities.’ Now the PERSON once again has confidence and self-esteem, empowerment and is more able to take control over her own life. Personhood has returned.
Summary
Alois Alzheimer described the disease back in 1906. In 2020, even though we have no immediate cure for the neurocognitive disorders, there is much more hope; many more positive interventions; much more knowledge and thus it is no longer all doom and gloom!
My book, A Clinician’s Guide to Non-Pharmacological Dementia Therapies, is geared towards the use of approaches, techniques and interventions that are based on the psychosocial model. The way I view this is model is by providing interventions that support, and work in collaboration with, the medical model.
One of the areas explored in the book is the use of hypnotherapy with people living with a neurocognitive disorder. Following research which I led in the UK, we were able to demonstrate that hypnotherapy improves 7 key areas: Concentration, Relaxation, Motivation, Activities of Daily Living, Immediate memory, Memory for significant events and socialization. As you will agree, these are areas that have a huge impact on the symptoms of the disease.
Other strategies include the use of Cognitive Behaviour Therapy, Intensive Ranch and Farm Retreat Therapy and The Nightingale Model of Enriched Care.
Get your copy of A Clinician’s Guide to Non-Pharmacological Dementia Therapies, here.
You can also learn more about Dr Daniel J. Nightingale’s latest book, The Pocket Guide to Mouth and Dental Hygiene in Dementia Care, here.